Basic concepts and terminology Two major processes involved in cell growth: Proliferation: the growth or production of cells by multiplication Differentiation: cellular differentiation is the process by which a less specialized cell becomes a more specialized cell type. Cancer is a disease of abnormal growth. When the growth and development of normal cell loses control, tumor cells begin to appear, which is called tumorigenesis.
Benign versus malignant. Metastasis. Staging. Clinical utilities of tumor markers. Examples of tumor markers and their uses.
Two major processes involved in cell growth: Proliferation: the growth or production of cells by multiplication. Differentiation: cellular differentiation is the process by which a less specialized cell becomes a more specialized cell type. Cancer is a disease of abnormal growth. When the growth and development of normal cell loses control, tumor cells begin to appear, which is called tumorigenesis.
According to the American Cancer Society, cancer is a group of diseases characterized by uncontrolled growth and spread of abnormal cells. It consists of more than 100 different diseases. Cancer can arise in many sites and behave differently depending on its organ of origin. Cancer is an abnormal, continuous multiplying of cells. The cells divide uncontrollably and may grow into adjacent tissue or spread to distant parts of the body. The mass of cancer cells eventually become large enough to produce lumps, masses, or tumors that can be detected.
Neoplasia and hyperplasia are two similar biologic processes. Hyperplasia involves the multiplication of cells in an organ or tissue, which may consequently have increased in volume. Neoplasia involves the possibility of normal cells undergoing cancerous proliferation as hyperplasia taking place under less controlled conditions; it is, therefore, a form of pathologic hyperplasia. The major difference between them is how growth is controlled. Hyperplasia serves a useful purpose and is controlled by stimuli, whereas neoplasia is unregulated and serves no purpose. The elevation of tumor marker in the case of the hyperplasia will be transient, whereas neoplasia will be long lasting phenomena.
1. Abnormality. Cells are the structural units of all living things. trillions of cells are found in human, Cells carry out all kinds of functions of life: the beating of the heart, breathing, digesting food, thinking, walking, and so on. However, all of these functions can only be carried out by normal healthy cells. Some cells stop functioning or behaving as they should serving no useful purpose in the body at all, and become cancerous cells.
2. Uncontrollability. The most fundamental characteristic of cells is their ability to reproduce themselves. They do this simply by dividing. The division of normal and healthy cells occurs in a regulated and systematic fashion. In most parts of the body, the cells continually divide and form new cells to supply the material for growth or to replace injured cells. For example, when you cut your finger, certain cells divide rapidly until the tissue is healed and the skin is repaired. They will then go back to their normal rate of division. In contrast, cancer cells divide in a random manner. The result is that they typically go into a non-structured mass or tumor.
3. Invasiveness. Tumors destroy the part of the body in which they originate and then spread to other parts where they start new growth and cause more destruction invasive cancer. This characteristic distinguishes cancer from benign growths, which remain in the part of the body in which they start. Although benign tumors may grow quite large and press on neighboring structures, they do not spread to other parts of the body. Frequently, they are completely enclosed in a protective capsule of tissue and they typically do not pose danger to human life like malignant tumors.
Although cancer is often referred to as a single condition, it actually consists of more than 100 different diseases. Cancer can arise in many sites and behave differently depending on its organ of origin. Breast cancer, for example, has different characteristics than lung cancer. Cancer originating in one body organ takes its characteristics with it even if it spreads to another part of the body. For example, metastatic breast cancer in the lungs continues to behave like breast cancer when viewed under a microscope, and it continues to look like a cancer that originated in the breast.
In western societies one death in five is caused by cancer. The effects of tumor growth may be local or systemic. E.g. obstruction of blood vessels, lymphatics or ducts, damage to nerves, effusions, bleeding, infection, necrosis of surrounding tissues and eventually death of the patient. The cancer cells may secrete toxins locally or into the general circulation. Both endocrine and non-endocrine tumors may secrete hormones or other regulatory molecules.
The local growth of a tumor can cause a wide range of abnormalities in commonly requested biochemical tests. This may be a consequence of obstruction of blood vessels or ducts. e.g. the blockage of bile ducts by carcinoma of head of pancreas causes elevated serum alkaline phosphatase and sometimes jaundice. The liver is often the site of metastatic spread of a tumor. Metastatic spread of a tumor to an important site may precipitate complete system failure. For example, destruction of the adrenal cortex by tumor causes impaired aldosterone and cortisol secretion.
Rapid tumor growth gives rise to abnormal biochemistry. Leukemia and lymphoma are often associated with elevated serum urate concentrations. Serum lactate dehydrogenase is often elevated. Large tumor may cause lactic acidosis. Renal failure may occur in patients with malignancy for the following reasons: obstruction of the urinary tract. hypercalcemia. Bence-Jones proteinuria. hyperuricemia. nephrotoxicity of cytotoxic drugs.
Cancer cachexia: bad condition describes the wasting characteristics that are usually seen in cancer patients like weight loss, wasting of muscle, loss of appetite, and general debility that can occur during a chronic disease) The features include anorexia, lethargy, weight loss, muscle weakness, anemia and pyrexia. The development of cancer cachexia is due to many factors and is incompletely understood. inadequate food intake. impaired digestion and absorption. competition between the host and tumor for nutrients. The growing tumor has a high metabolic rate and may deprive the body of nutrients. One consequence of this is a fall in the plasma cholesterol level in cancer patients. increased energy requirement of the cancer patients. The host reaction to the tumor is similar to the metabolic response to injury, with increased metabolic rate and altered tissue metabolism. Certainly, there is an imbalance between dietary calories intake and body requirements.
The observation that small tumors can have profound effect on host metabolism suggests that cancer cells secrete or cause the release of humoral agents that mediate the metabolic changes of cancer cachexia. Some of these, such as tumor necrosis factor, have been identified.
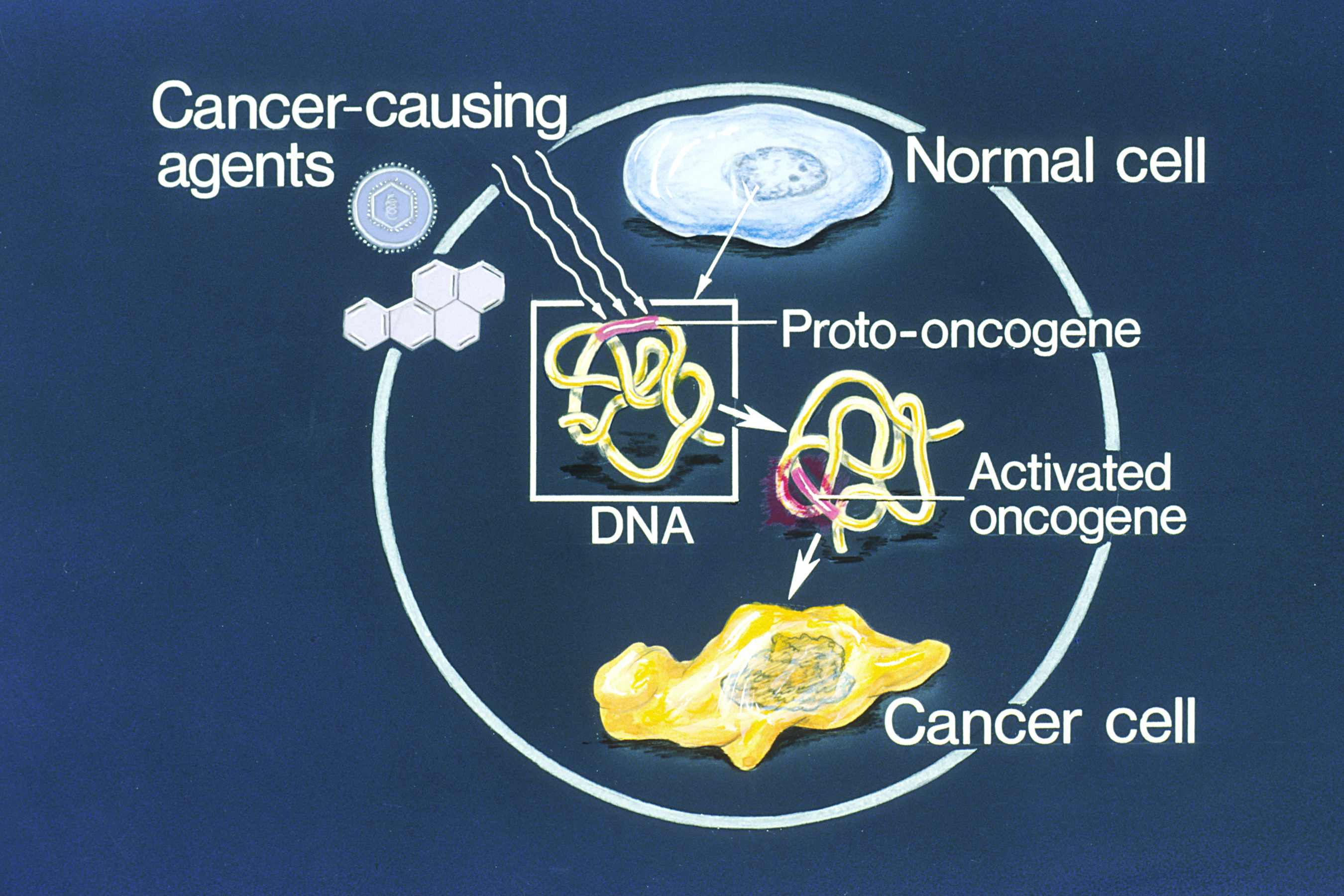
When either differentiation or proliferation becomes unregulated, there is a risk for normal cells to be converted into cancer cells. This process is usually associated with changes of the genetic components of the cell. Changes include: Mutation of cellular oncogenes (oncogene is a gene that, when mutated or expressed at high levels, helps turn a normal cell into a tumor cell) abnormal regulation of their expression. rearrangements of oncogenic DNA sequences (oncogenic: describing a substance, organism, or environment that is known to be a casual factor in the production of a tumor. Some animal viruses are known to be oncogenic; others are suspected of being so in man, including some papovaviruses, adneviruses, and herpesviruses.
Most tumor cells undergo a benign stage, gradually progress to malignancy, and eventually become metastasized if not treated. The genetic instability associated with tumor cells can make tumor cells more susceptible to additional mutations, which may ultimately lead to malignant disease. During the benign stage, tumors remain at the primary site and present a smaller risk to the host. At this stage, the patient stands a good chance of being treated, such as by complete removal of tumor the early detection of a benign tumor is critical to cancer prevention in general and to high-risk families in particular. All benign tumors are well differentiated and composed of cells resembling the mature normal cells from the tissue of origin of the neoplasm.
Benign tumors: are not cancerous. can usually be removed. do not come back in most cases. do not spread to other parts of the body, and the cells do not invade other tissues. Malignant tumors: are cancerous. can invade and damage nearby tissues and organs. metastasize (cancer cells break away from a malignant tumor and enter the bloodstream or lymphatic system to form secondary tumors in other parts of the body)
Metastasis is a multistep processes involving numerous tumor cell-host cell and cell-matrix interactions. For tumor cells to metastasize: the tumor cells at the primary site have to first penetrate their adjacent surroundings, including the epithelial basement membrane and the stroma. they then invade blood or lymphatic vessels and are carried to distant sites, until they are finally arrested in the venous/capillary beds or solid tissue of a distant organ. in this new environment, these tumor cells must again penetrate the vascular walls to proliferate at the new distant site.
In general, the larger, more aggressive, or more rapidly growing the primary neoplasm, the greater the likelihood that the tumor cells will metastasize. Metastasis is highly selective process. Cells isolated from individual tumors may differ in many ways: with respect to capacity for invasion and metastasis. growth rate. cell surface receptors. immunogenicity. response to cytotoxic drugs.
The pathway of signal transduction controls both cell cycle and apoptosis. The pathway is an orderly and specific transmission of growth-regulatory messages from outside the cell to the machinery controlling replication inside the cell nucleus. On binding of the stimulus to the receptor, the transmission of signal is carried out by protein phosphorylation involving activation of the enzymatic function of many kinases. These stimuli include hormones, insulin, cytokines, epidermal growth factor and others.
Cell cycle is tightly regulated and controlled with different factors( Cyclin A, Cyclin-dependent kinases: CDK2, Cyclin D1 , CDK4 and others. Tumors results from the absence of certain cell cycle controls. Defects in the cell cycle machinery may, therefore, help cause cancer.
Apoptosis, a programmed cell or physiologic death, is a natural self-destruct system present in all cells. Failure of cells to undergo apoptotic cell death may lead to cancer. It is a natural process the body employs for the replacement of cells and the deletion of damaged cells. Apoptosis is a control mechanism for tissue remodeling during growth and development apoptosis provides a way for the body to eliminate cells that have developed improperly, or that have sustained genetic damage.
A tumor must continuously stimulate the growth of new capillary blood vessels for the tumor to grow. Angiogenesis is critical, not only for growth of cancer mass but also for the shedding of primary cells from the primary tumor and development of metastases.
Carcinomas are cancers that occur in epithelial surfaces; the cells that form the outer surface of the body to line or cover the body s cavities, tubes and passageways. Adenocarcinomas are cancers that form on a glandular surface, such as the lung, breast, prostate, ovary, or kidney. Sarcomas are cancers that occur in supporting structures, such as bone, muscle, cartilage, fat, or fibrous tissue. Leukemias and lymphomas are cancers that occur in blood cell elements. Brain cancers, nerve cancers, melanomas, and certain testicular and ovarian cancers do not fall into this general categories.
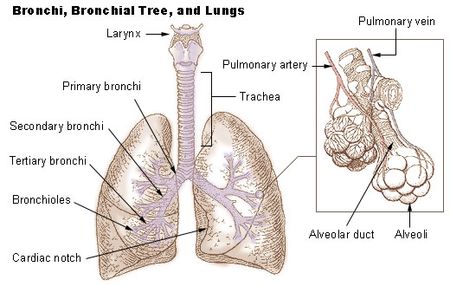
Some cancers secrete hormones, even though the tumor has not arisen from an endocrine organ Referred as ectopic hormone production, Small cell carcinomas (Common malignant neoplasm of bronchus) are the most aggressive of the lung cancers and are associated with ectopic hormone production Ectopic ACTH secretion (Adrenocorticotropic hormone secreted by the anterior pituitary gland and stimulate androgens and cortisol release from the adrenal cortex causing Cushing’s syndrome. Patients with malignancy develop SIAD (syndrome of inappropriate antidiuretic hormone). High levels of ADH water is retained and patients present with hyponatremia. This is probably the commonest biochemical abnormality seen in patients with cancer and is almost invariably due to pituitary ADH secretion in response to non-osmotic stimuli. Some cancers may cause hypercalcemia. In many cases this is due to the secretion of parathyroid hormone related protein (PTHrP), so-called because of its relationship with PTH in its structure and function.
A biopsy is examined microscopically. Low grade: slow growing, well differentiated, less aggressive, and less likely to spread quickly. Intermediate grade. High grade: fast growing, poorly differentiated, tend to be more aggressive , and are more likely to spread quickly. Grading systems differ depending on the type of cancer. For example, breast cancers are graded 1, 2 or 3 which is much the same as low, intermediate and high grade. Another example is prostate cancer which is graded by a Gleason Score.
In addition to clinical examination, a variety of imaging and surgical techniques may be employed to provide a more accurate assessment. Stage 0 or carcinoma in situ: Carcinoma in situ is very early cancer. The abnormal cells are found only in the first layer of cells of the primary site and do not invade the deeper tissues. Stage I: Cancer involves the primary site, but has not spread to close tissues. Stage IA: a very small amount of cancer: visible under a microscope and is found deeper in the tissues. Stage IB: a larger amount of cancer is found in the tissues.
Stage IIB: cancer has spread to other tissue around the primary site. Stage III : Cancer has spread throughout the nearby area. Stage IV: Cancer has spread to other parts of the body. stage IVA: cancer has spread to organs close to the pelvic area. stage IVB: cancer has spread to distant organs, such as the lungs. Recurrent: Recurrent disease means that the cancer has come back (recurred) after it has been treated.
Tumor markers are substances that can be detected in higher-than-normal amounts in the blood, urine, or body tissues of some patients with certain types of cancer. Tumor markers are produced either by the body in response to the presence of cancer or certain benign (non-cancerous) conditions or by the tumor itself. Their measurement or identification is useful in patient diagnosis or clinical management. A tumor marker has been secreted or released by the tumor cells. Such markers are not necessarily unique products of the malignant cells, but may simply be expressed by the tumor in a greater amount than normal cells. The ideal marker would be. a blood test for cancer. a positive result would occur only in patients with malignancy, one that would correlate with stage and response to treatment. that was easily and reproducibly measured. No tumor marker now available has met this ideal.
Tumor markers are molecules occurring in blood or tissue that are associated with cancer and whose measurement or identification is useful in patient diagnosis or clinical management. The ideal marker would be: a blood test for cancer in which a positive result would occur only in patients with malignancy. would correlate with stage and response to treatment. easily and reproducibly measured. No tumor marker now available has met this ideal.
Tumor markers can be used for one of the following purposes: 1. Screening a healthy population or a high risk population for the presence of cancer even that most tumor markers, lack specificity and sensitivity. 2. Monitoring the course in a patient in remission or while receiving surgery, radiation, or chemotherapy gives an indication of the effectiveness of antitumor drug used. 3. Detection of recurrence following surgical removal of the tumor Because patients being monitored have already had their cancer identified, the specificity of the tumor marker is less important than sensitivity. The sensitivity is important to detect recurrence as early as possible.
4. Determining the prognosis in a patient is usually based on tumor aggressiveness: a. determine how a patient should be treated. b. indicate risk and predict the length of a relapse-free. c. survival period at the time of primary therapy. 5. early detection and making an early diagnosis of cancer or of a specific type of cancer allows the detection of early neoplasms at the curable stage. No test meets all of those requirements.
Include markers defined by both monoclonal antibodies and polyclonal antisera, called oncofetal antigens. The oncofetal substances, present in embryo or fetus, diminish to low levels in the adult but reappear in the tumor. Carcinoembryonic Antigen (CEA) The CEA was one of the first oncofetal antigens to be described and exploited clinically. It is a complex glycoprotein that is associated with the plasma membrane of tumor cells. CEA is a normal cell product that is over-expressed by adenocarcinomas, primarily of the colon, rectum, breast and lung. CEA is the most widely used tumor marker for gastrointestenal cancer (colon) Elevated CEA levels are found in a variety of cancers colon, pancreatic, gastric, lung, and breast cancer. It is normally found in small amounts in the blood of most healthy people but may become elevated in people who have cancer or certain benign conditions.
Elevated CEA levels can also occur in patients with non-cancerous conditions, including inflammatory bowel disease, pancreatitis and liver disease, chronic lung disease, cirrhosis. The CEA was found to be elevated in up to 19 percent of smokers and in 3 percent of a healthy control population. The test for CEA cannot substitute for a pathological diagnosis. As a screening test, the CEA is also inadequate. The CEA has been suggested as having prognostic value for patients with colon cancer. CEA values have been positively correlated with stage and negatively correlated with disease free survival. The CEA is of some use as a monitor in treatment. Usually the CEA returns to normal within 1 to 2 months of surgery,
It is a major component of fetal plasma, reaching a peak concentration of 3 mg/ml at 12 weeks of gestation. Following birth, it clears rapidly from the circulation, having a half life of 3.5 days, and its concentration in adult serum is less than 20 ng/ml. AFP is of importance in diagnosing hepatocellular carcinoma and may be useful in screening procedures. An elevated AFP has been termed the single most discriminating laboratory test indicative of malignant disease now available it could be valuable in screening for hepatocellular carcinoma in high risk populations.
The AFP is less frequently elevated in other malignancies such as pancreatic cancers, gastric cancers, colonic cancers, and bronchogenic cancers. This elevation was not necessarily associated with liver metastases. The AFP is rarely elevated in healthy persons, and a rise is seen in only a few disease states like liver diseases, viral or drug induced hepatitis. Thus, AFP is a useful marker in hepatocellular carcinoma and germ cell tumors. The AFP is high in the first trimester of gestation and in the case of the presence of neural tube defect. Newborn have much higher serum AFP than adults.
It is defined by a monoclonal antibody (OC125) that was generated by immunizing laboratory mice with a cell line established from human ovarian carcinoma. It circulates in the serum of patients with ovarian carcinoma and investigated for possible use as a marker. The level CA125 correlates with patient response to treatment of ovarian cancer. The CA125 is elevated in other cancers including uterus, cervix, pancreatic, lung, breast, and colon cancer, and in menstruation, pregnancy, and other gynecologic and non gynecologic conditions. Changes in CA 125 levels can be used effectively in the management of treatment for ovarian cancer. CA 125 levels can also be used to monitor patients for recurrence of ovarian cancer.
CA19-9 is defined by monoclonal antibody generated against a colon carcinoma cell line to detect a mono sialo-ganglioside found in patients with gastrointestinal adenocarcinoma. It is found it to be elevated in 21 to 42 percent of cases of gastric cancer, 20 to 40 percent of colon cancer, and 71 to 93 percent of pancreatic cancer, and has been proposed to differentiate benign from malignant pancreatic disease. CA 19-9 has also been identified in patients with hepatocellular cancer and bile-duct cancer. Non-cancerous conditions that may elevate CA 19-9 levels include gallstones, pancreatitis, cirrhosis of the liver, and cholecystitis. CA 19-9 can be used in monitoring of the patients and recurrent cancer.
PSA is tissue specific tumor marker; it is found in normal prostatic epithelium and secretions but not in other tissues. It is a glycoprotein, whose function may be to lyse the seminal clot. PSA is highly sensitive for the presence of prostatic cancer. The elevation correlated with stage and tumor volume. It is predictive of recurrence and response to treatment. PSA is the first tumor marker recommended for screening of prostate cancer in men older than age 50. It found in two major forms: free form and PSA-α-antichymotrypsin (PSA-ACT) complex. Measuring the ratio between the free and complexes of PSA helps to differentiate benign prostate hyperplasia from prostate cancer. Age Range (Years) Caucasians [ng/ml]
a natural product of affected cells by cancer: Insulin production by islet cell tumor, Calcitonin by medullary thyroid carcinoma, Catecholamines by pheochromocytoma. The hormone is not a natural product of its associated organ, in which case is designated ectopic . Examples include the production of ACTH and ADH by lung cancers.
In cancers of the parafollicular C cells, called medullary carcinomas of the thyroid, levels of this hormone are elevated. Calcitonin is one of the rare tumor markers that can be used to help diagnose early cancer. Because medullary carcinoma of the thyroid is often inherited, blood calcitonin can be measured to detect the cancer in its earliest stages in family members who are at risk. Other cancers, particularly lung cancers, can produce calcitonin, but measurement of its level in the blood is not usually used to follow these cancers.
HCG is a glycoprotein consisting of subunits α and β, which are nonconvalently linked. The hormone is normally produced by the trophoblastic cells of the placenta and is elevated in pregnancy. hCG is elevated in the urine and serum during the pregnancy. Its most important uses as a tumor marker are in gestational trophoblastic disease (a group of rare pregnancy-related tumours) and germ cell tumors of ovary and testis. Gestational trophoblastic disease is proliferation of trophoblastic tissue in pregnant causing excessive uterine enlargement, vomiting, vaginal bleeding, diagnosis includes measurement of the β hCG.
All gestational trophoblastic tumors produce HCG, and it is a valuable marker in these tumors, HCG is extremely sensitive, being elevated in women with minute amounts of tumor. Free β- HCG is occasionally elevated in ovarian cancer and lung cancers breast, lung, and gastrointestinal tract, but in these diseases it has found little clinical application. Free β- HCG is sensitive and specific for aggressive neoplasmas.
Thyroglobulin is elevated in many thyroid diseases. When a thyroid cancer is surgically removed, the whole thyroid gland is usually also removed. Therefore, any elevation of the thyroglobulin level above 10ng/ml suggests that the cancer has returned. Metastatic thyroid cancer. It is used to evaluate the effectiveness of treatment for thyroid cancer and to monitor for recurrence.
Enzymes. Enzymes that can be used as markers are either native to normal tissue or associated with changes in metabolism that are unique to cancer tissue. Neuron Specific Enolase. Neuron specific enolase is an isozyme of the glycolytic pathway that is found only in brain and neuroendocrine tissue. It is an immunohistochemical marker for tumors of the central nervous system, neuroblastomas. NSE has been detected in patients with neuroblastoma, small-cell lung cancer, Wilms tumor (nephroblastoma; tumor of kidney), melanoma, and cancers of the thyroid, testicle and pancreas. NSE as a tumor marker has concentrated primarily on patients with neuroblastoma and small-cell lung cancer.
Galactosyl Transferase II, an isozyme of galactosyl transferase, has been shown to be elevated in a variety of malignancies, predominantly gastrointestinal. In colon cancer its level correlated with the extent of disease and disease progression; In pancreatic cancer it was more sensitive and specific in distinguishing benign from malignant disease than CEA and other tests. Prostatic acid phosphatase. It is capable of monitoring prostate malignancy. It is rarely used now, because the PSA test is much more sensitive.
ALP has been used to detect mainly malignancies in bone and liver and to detect metastases to these organs. Osteoblastic lesions in the bone produced by prostate cancer metastases give rise to enormous elevations in ALP, Whereas lesions produced by metastatic breast cancer cause only mild or no elevation. Other causes of elevated ALP include extrahepatic obstruction of the bilialy tract, which usually results in a twofold increase in ALP levels. Diseases such as leukemia that infiltrate the liver can cause marked elevations in ALP levels. The source of the elevated ALP (bone or liver) can be identified by measuring other liver enzymes, such as gamma-glutamyl-transferase and or by measuring ALP activity.
CK-BB (CKl) is found in the brain, gastrointestinal tract, uterus, and prostate. Elevations of CK-BB (and total CK) can be found in prostatic carcinoma and metastatic cancer of the stomach. Immunoglobulins. Production of a monoclonal immunoglobulin molecule is characteristic of multiple myeloma. Bence Jones protein (paraproteins) are usually complete antibody molecules but may be isolated light chains or, rarely, heavy chains. They may be lambda or kappa light chains and of any immunoglobulin subtype. Bence Jones protein found in high concentration in serum and in urine. Immunoglobulins are valuable in the staging and treatment of myeloma, the amount of paraprotein serving as an index of tumor volume.
These intracellular receptors are measured directly in tumor tissue. Most oncologists have used the estrogen and progesterone receptors not only to predict the probability of response to hormonal therapy at the time of metastatic disease, but also to predict the likelihood of recurrent disease. These receptors are also used to predict the need for adjuvant hormonal therapy or chemotherapy. The measurement of estrogen and progesterone receptors in biopsy material has been used to determine which breast cancer patients will respond to endocrine therapy, e.g. with the antiestrogen tamoxifen.
Cancers show low (left), moderate (center), or high (right) proportions of receptor-containing cells. ×
The most prominent of these are the genes for susceptibility to breast and ovarian cancer, such as BRCA1 and BRCA2. BRCA1 & BRCA2 (breast cancer 1 & 2): Are human genes belong to a class of genes known as tumor suppressors, some mutations of which are associated with a significant increase in the risk of breast cancer, as well as other cancers. Screening tests for BRCA1 and BRCA2 are now available to screen these families for the identification of carriers.
Tumor-marker levels can be elevated in people with benign conditions. Tumor-marker levels are not elevated in every person with cancer, especially in the early stages of the disease. Many tumor markers are not specific to a particular type of cancer. The level of a tumor marker can be elevated by more than one type of cancer.
Marker. Tumor. Screening. Diagnosis. Prognosis. Monitoring. Follow-up. AFP. Germ cell. AFP. Hepatoma. HCG. Germ cell. HCG. Choriocarcinoma. CA 125. Ovarian. Acid phosphatPSA. Prostate. Prostate. CEA. Colorectal. Calcitonin. Medullary carcinoma of thyroid. Hormones. Endocrine. Paraproteins. Myeloma.
Liver carcinoma: -fetoprotein. Ovarian carcinoma: CA 125. Colorectal cancer: CA Pancreatic carcinoma: amylase, CEA (in case of liver metastasis) Breast cancer: BRACA1, BRAC2. Prostate cancer: PSA (total and free). Most PSA in the blood is bound to serum proteins. A small amount is not protein bound and is called free PSA. In men with prostate cancer the ratio of free (unbound) PSA to total PSA is decreased. The risk of cancer increases if the free to total ratio is less than 25%. Non specific marker: hCG.
(1) Screening a healthy population or a high risk population for the presence of cancer. (2) Making a diagnosis of cancer or of a specific type of cancer. (3) Determining the prognosis in a patient; (4) Monitoring the course in a patient in remission or while receiving surgery, radiation, or chemotherapy. No test meets all of those requirements. The reason for this is the relative lack of sensitivity and specificity of the available tests. Tumor markers include many substances that are not readily systematically organized. These are not unique to cancer cells; but they represent unusual tumor production of a normal element. Some markers are produced by the organism in response to the cancer s presence.
tumor-marker levels may reflect the extent or stage of the disease. can be useful in predicting how well the disease will respond to treatment. A decrease or return to normal in the level of a tumor marker may indicate that the cancer has responded favorably to therapy. A rise in the tumor-marker level may indicate that the cancer is spreading. Additionally, measurements of tumor-marker levels may be used after treatment has ended as a part of follow-up care to check for recurrence.
CA 15-3 cannot be used to screen or diagnose patients with breast cancer because of low detection rate in early stages. It has been widely used to monitor the effectiveness of treatment for metastatic cancer. CA 15-3 levels may iraised by cancers of the ovary, lung, and prostate. Elevated levels of CA 15-3 may be associated with non-cancerous conditions, such as benign breast or ovarian disease, endometriosis, pelvic inflammatory disease, and hepatitis. Similar to the CA 15-3 antigen, CA is found in the blood of most breast cancer patients. CA levels can also be elevated by cancers of the colon, stomach, kidney, lung, ovary, pancreas, uterus and liver. Non-cancerous conditions that can also elevate CA levels include first-trimester pregnancy, endometriosis, ovarian cysts, benign breast disease, kidney disease and liver disease.

JPM, Free Full-Text
Biomedicines, Free Full-Text
Lung Cancer - Physiopedia

Cardiac Endocrinology: Heart-Derived Hormones in Physiology and
Tumor Markers Basic concepts and terminology Cancer - ppt download
Oncogene - Wikipedia

Tumor markers

Biomarkers in cancer

Towards Immunotherapy for Pediatric Brain Tumors: Trends in Immunology